

In this review, we discuss the need to return to the ‘renaissance’ of electrophysiology (EP) when His bundle and electrical conduction system recordings were the focus of invasive study. Identifying patients who might achieve physiological resynchronisation, however, can be challenging. Indeed, the goal of CRT more broadly should be complete physiological resynchronisation utilising the His–Purkinje system, if possible. The physiology of conduction system disease is highly individualised and requires therapy directed at the patient’s underlying pathophysiology traditional LV lead placement into an available tributary of the coronary sinus might not meet the needs of an individual patient. 11–14 Non-response is not necessarily a failure of biventricular pacing, but rather a failure in appropriate patient selection. Research has shown that patients with LBBB are the most likely to benefit from CRT, and that patients without significant LV conduction delay, particularly those with right bundle branch (RBBB) or non-specific intraventricular conduction delay (IVCD), derive little to no benefit from biventricular pacing. 8–10 During the past decade, we have gained a deeper mechanistic understanding of the benefits of biventricular pacing.

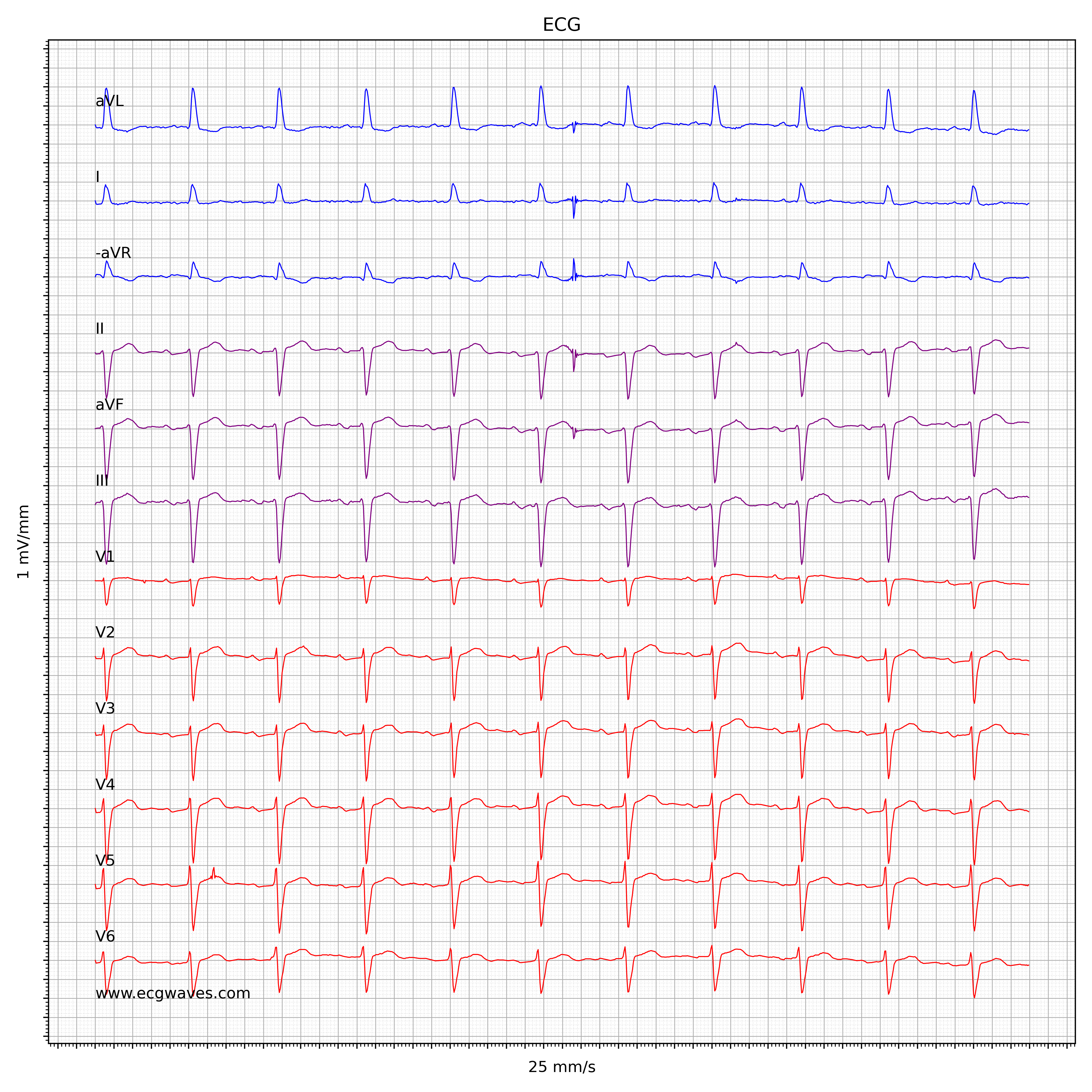
2–7 However, despite these significant benefits, up to one-third of patients do not improve after biventricular pacing, and the overall rate of response from traditional biventricular pacing has remained stagnant despite technical improvements in lead delivery and site selection. These abnormal electrical activation patterns, particularly the left bundle branch block (LBBB) pattern, are associated with the presence, development or worsening of cardiomyopathy, and leads to increased risk of subsequent morbidity and mortality.Ĭardiac resynchronisation therapy (CRT) via biventricular pacing has been established as the mainstay electrical pacing modality to reverse the deleterious effects of electromechanical dyssynchrony, with significant reductions in mortality and heart failure (HF) hospitalisation for patients with wide QRS, as shown in multiple randomised controlled trials. fascicular blocks or bundle branch blocks). When normal transit through the His–Purkinje system is disrupted, stereotypic conduction block patterns are manifested on the 12-lead surface ECG (e.g. 1 The rapid and synchronous activation of the LV through the specialised His–Purkinje network is highly intricate and efficient, preserving normal physiological coupling between electrical excitation and mechanical contraction. recorded the total excitation of the human heart with 870 electrodes and confirmed the first 10 ms of left ventricular (LV) activation as trifascicular in nature. Left-sided EPS has the potential to refine patient selection in CRT trials and may be used to physiologically phenotype distinct conduction patterns beyond LBBB pattern. Future EPS are required to determine the impact of newer approaches to conduction system pacing, including intraseptal or left ventricular septal pacing. Patients with intact Purkinje activation and intraventricular conduction delay are less likely to benefit from HBP. During a novel extension of the classical EPS to involve left-sided recordings, we found that conduction block associated with the LBBB pattern is most often proximal, usually within the left-sided His fibres, and these patients are the most likely to demonstrate QRS correction with HBP for resynchronisation. The determination of LBBB pattern is conventionally made by assessment of surface 12-lead ECGs and can include patients with and without conduction block, as assessed by invasive electrophysiology study (EPS). The ability to normalize wide QRS patterns with His bundle pacing (HBP) has called this notion into question. One historical presumption of LBBB has been that the underlying pathophysiology involved diffuse disease throughout the distal conduction system. Left bundle branch block (LBBB) is associated with improved outcome after cardiac resynchronisation therapy (CRT).


 0 kommentar(er)
0 kommentar(er)
